Anosmia and ageusia as clinical manifestation of COVID-19
Virginia Thornley, M.D.s
Neurologist
April 24, 2020
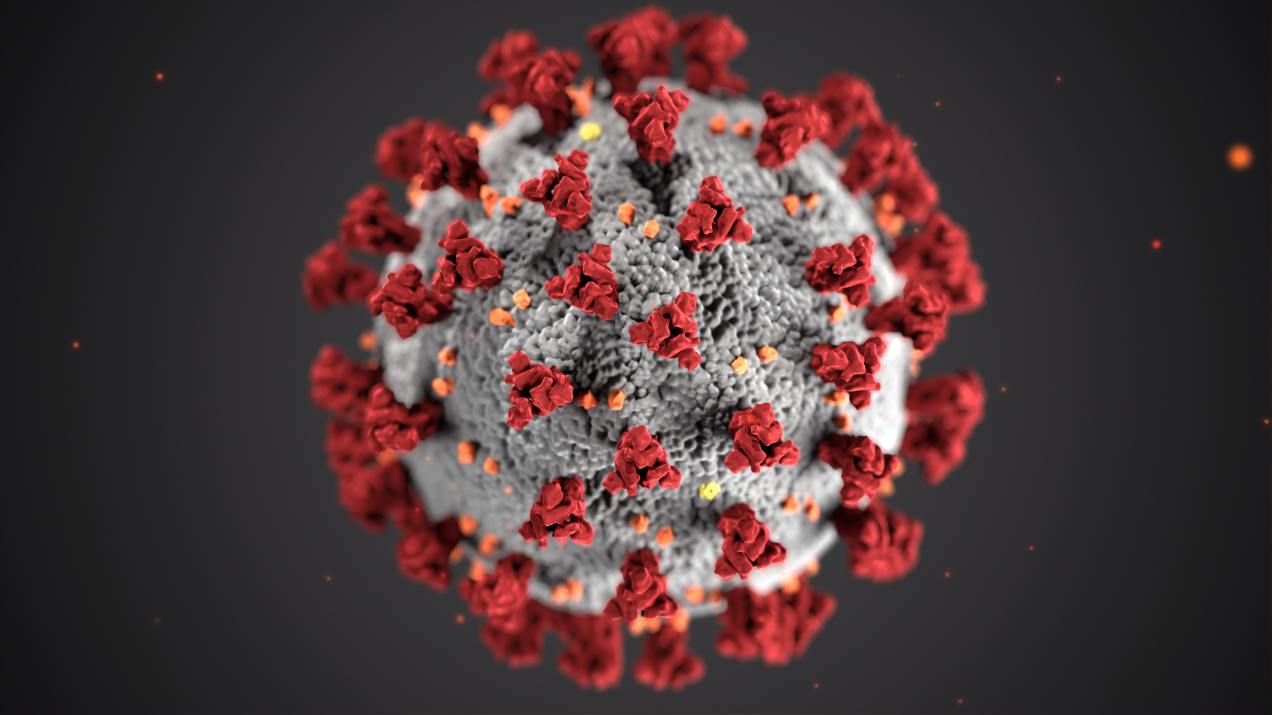
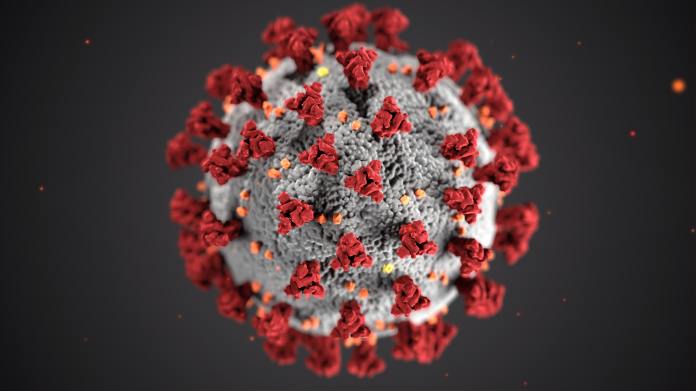
photo credit CDC by Unsplash
Neurologybuzz.com
http://virginiathornleymd.com/
Introduction
COVID-19 can present with a variety of symptoms and is not necessarily limited to fever and respiratory symptoms. As the pandemic continues, more observations of the wide spectrum of clinical presentations are seen. Two of these are anosmia and ageusia-loss of smell and taste.
Studies
A very recent study came out April 22, 2020, comparing patients with COVID-19 and influenza with 79 cases including 40 controls. New onset smell and taste disorders (STD) were found to be more common as initial clinical symptoms compared to controls with influenza (1). In the group with COVID-19, 35% had acute onset as the first symptom, 70% had loss of smell, 90% had loss of taste, and 12.9% had nasal obstruction. 40% recovered after 7.4 days(1).
Anosmia or lack of smell has been reported in several countries U.K., France, United States, South Korea, Italy and Iran (2).
There are case reports on 2 patients with COVID-19 infection one who died, showing anosmia in the absence of respiratory symptoms. It is thought to be related to inflammation of the olfactory nerves (3).
Conclusion
There are now randomized controlled clinical studies showing that anosmia and ageusia can be an initial clinical symptom of COVID-19. There are case reports that it can be the only symptom.
Disclaimer: Information only not advice talk to your doctor.
Neurologybuzz.com
References
1. Beltram-Corbelliini, A., Chico-Garcia, J.L, Martinez-Poles, J., Rodrigiez-Jorge, F., Natera-Villalba, E., Gomez,Corral, J., Gomez-Lopez, A., Monreal, E., Parrra-Diaz, P., Cortes-Cuevas, J.L, Galan, J.C., Fragola-Arnau, C., Porta-Etessam, J., Masjuan, Alonso-Canovas, A., Acute-onset small and taste disorder in the context of COVID-19: a pilot multi-center PCR-based case-control study. Eur J Neurol 2020 Apr 22. doi: 10.1111/ene.14273
2. Heidari, F., Karimi, E., Firouzifar, M., Khamushian, P., Ansari, R., Mohammed Ardehali, Heidari, F. Rhinology, 2020, Apr 22. doi: 10.4193/Rhin20.140
3. Villalba, N.L., Maouche, Y., Ortiz, M.B.A., Sosa, Z.C., Chahbazia, J.B., Syrovatkova, A., Pertoldi, P., Andres, E., Abrar-Ahmed, Z, Anosmia and dysgeusia in the absence of other respiratory diseases: should COVID-19 infection be considered? Eur J Case Rep Intern Med. 2020. 7(4):001641 doi: 10.12890/2020_001641