Review of literature: introduction to the COVID19 and clinical presentations
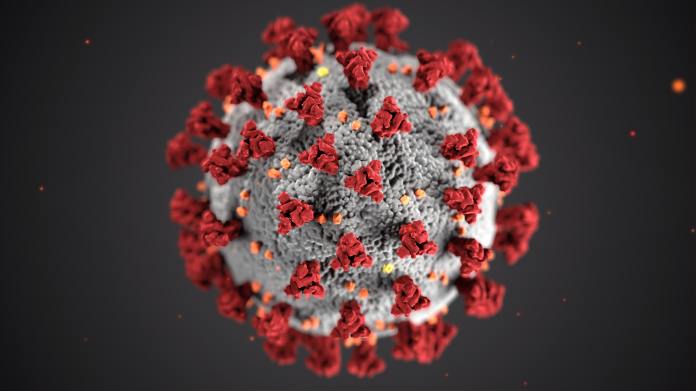
credit: photo by CDC by Unsplash
Virginia Thornley, M.D.
Neurologist
April 2, 2020
Introduction
A new virus emerged in Wuhun, China in December 2019. But the information is still emerging on how to treat it and the exact pathophysiology.
The coronavirus is a type of virus that can infect both animals and humans.
It was named COVID19 for corona virus disease 2019 and renamed SARS-CoV2 which was discovered in the epithelium of the respiratory system of patients from Wuhun, China (1).
COVID-19
COVID19 first occurred December 7, 2019 in the markets of Wuhun, China. The pathogen is the SAR-CoV2. The intermediate host is thought to be the Pangolin. It is a type of RNA virus. The original host is an animal but it jumped to humans. The species pathogen is the B-corona virus. The latency period is about 2-7 days infecting people who have never been exposed to it before(1).
Clinical presentation
The infection is classified as mild, moderate, severe and critical. Mild cases present with fever, respiratory symptoms and no pneumonia on imaging studies. Moderate is described as those with fever, respiratory symptoms and pneumonia on imaging studies. Severe cases present with respiratory failure with a respiratory rate greater than 30/minute, oxygen saturation or O2 saturation of less than or equal to 93mmHg, PaO2/FiO2 of less than 300mmHg. Critical cases include one of the following: need for mechanical ventilation, shock or organ failure requiring ICU admission. There can be dyspnea leading to acute respiratory distress syndrome (ARDS), metabolic abnormalities that are refractory to correction, shock and thrombosis(3).
Epidemiology
The SARS epidemic which occurred in 2003 affecting China extending to other other Southeast Asian countries, by contrast, lasted 7 months affecting 8096 people resulting in 774 deaths. There was a high mortality rate among hospital personnel of about 21% (1). The COVID19 started December 7, 2019 and is still ongoing at the time of this writing. At the time of this writing, there are 1,040617 affected with 55,188 deaths(2). The numbers continue to climb. It was declared a pandemic by the WHO. Most clinical cases are elderly, however, the coronavirus could be seen in those with diabetes mellitus and hepatitis B. An immunocompromised state is also a risk factor. Male to female ratio based on studies in China is 2.7:1. Mortality rate is 2.1%
References:
1. Xu, J., Zhao, S., Teng, T., Abdalla, A.E., Zhu, W., XIE, L., Wang, Y., Guo, X. Systematic Comparison of Two Animal-to-Human Transmitted Human Coronaviruses: SARS-CoV-2 and SARS-CoV. Viruses. 2020, Feb. 22;12(2).
2. Worldometer, Coronavurus pandemic 2019
3. Feng, Y., Liu, N., Hu, J., Wu, l., Su, G., Zhong, N., Zheng, Z. 4S Respiratory rehabilitation guidelines for patients with pneumonia infected by new Coronavirus. Chinese Journal of Tuberculosis and Respiratory Diseases, 2020, 43: Pre-published online. DOI: 10.3760 / cma.j.issn.1001-0939.2020.0004
Photo by CDC on Unsplash
Neurologybuzz.com